"Every Day And In Every Way I Am Getting Better And Better"...
.
.
.
Dehydration
| Dehydration Classification and external resources | |
| ICD-10 | E86. |
|---|---|
| ICD-9 | 276.5 |
Dehydration (HYPO-hydration) is the removal of water (hydro in ancient Greek) from an object. In Physiologic terms, it entails a relative deficiency of water molecules in relation to other dissolved solutes. Dehydration, thus, is slightly different from HYPO-volemia, which defines water deficiency only in terms of overall volume rather than in terms of solute concentrations.
Contents |
Medical causes of dehydration in humans
In humans, dehydration can be caused by a wide range of diseases and states that impair water homeostasis in the body. These include:
- External or stress-related causes
- Prolonged physical activity without consuming adequate water, especially in a hot and/or humid environment
- Prolonged exposure to dry air, e.g. in high-flying airplanes (5-15% relative humidity)
- Survival situations, especially desert conditions
- Blood loss or hypotension due to physical trauma
- Diarrhea
- Hyperthermia
- Shock (hypovolemic)
- Vomiting
- Burns
- Lacrimation
- Use of Methamphetamine and other stimulants.
- Malnutrition
- Electrolyte disturbance
- Hypernatremia (also caused by dehydration)
- Hyponatremia, especially from restricted salt diets
- Fasting
- Recent rapid weight loss may reflect progressive depletion of fluid volume (the loss of 1 L of fluid results in a weight loss of 1 kg or 2.2 lb).[1]
- Patient refusal of nutrition and hydration
- Electrolyte disturbance
- Other causes of obligate water loss
- Severe hyperglycemia, especially in Diabetes mellitus
Symptoms and prognosis
Symptoms may include headaches similar to what is experienced during a hangover, muscle cramps, a sudden episode of visual snow, decreased blood pressure (hypotension), and dizzinessfainting when standing up due to orthostatic hypotension. Untreated dehydration generally results in delirium, unconsciousness, swelling of the tongue[1] and in extreme cases death. or
Dehydration symptoms generally become noticeable after 2% of one's normal water volume has been lost. Initially, one experiences thirst and discomfort, possibly along with loss of appetite and dry skin. This can be followed by constipation. Athletes may suffer a loss of performance of up to 30%[2], and experience flushing, low endurance, rapid heart rates, elevated body temperatures, and rapid onset of fatigue.
Symptoms of mild dehydration include thirst, decreased urine volume, abnormally dark urine, unexplained tiredness, lack of tears when crying, headache, dry mouth, dizziness when standing due to orthostatic hypotension, and in some cases can cause insomnia.
In moderate to severe dehydration, there may be no urine output at all. Other symptoms in these states include lethargy or extreme sleepiness, seizures, sunken fontanel (soft spot) in infants, fainting, and sunken eyes.
The symptoms become increasingly severe with greater water loss. One's heart and respiration rates begin to increase to compensate for decreased plasma volume and blood pressure, while body temperature may rise because of decreased sweating. Around 5% to 6% water loss, one may become groggy or sleepy, experience headaches or nausea, and may feel tingling in one's limbs (paresthesia). With 10% to 15% fluid loss, muscles may become spastic, skin may shrivel and wrinkle, vision may dim, urination will be greatly reduced and may become painful, and delirium may begin. Losses greater than 15% are usually fatal. [3]
For adults over age 50, the body’s thirst sensation diminishes and continues diminishing with age. Many senior citizens suffer symptoms of dehydration. Dehydration along with hyperthermia results in seniors dying during extreme hot weather.
Dehydration is the excessive loss of water from the body. Diseases of the gastrointestinal tract can lead to dehydration in various ways. Often, dehydration becomes the major problem in an otherwise self-limited illness. Fluid loss may even be severe enough to become life-threatening.
Treatment
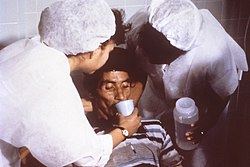
The best treatment for minor dehydration is drinking water and stopping fluid loss. Water is preferable to sport drinks and other commercially-sold rehydration fluids, as the balance of electrolytes they provide may not match the replacement requirements of the individual. To stop fluid loss from vomiting and diarrhea, avoid solid foods and drink only clear liquids.[4]
In more severe cases, correction of a dehydrated state is accomplished by the replenishment of necessary water and electrolytes (rehydration, through oral rehydration therapy or intravenous therapy). Even in the case of serious lack of fresh water (e.g., at sea or in a desert), drinking seawater or urine does not help, nor does the consumption of alcohol. It is often thought that the sudden influx of salt into the body from seawater will cause the cells to dehydrate and the kidneys to overload and shut down but it has been calculated that an average adult can drink up to 0.2 liters of seawater per day before the kidneys start to fail.
When dehydrated, unnecessary sweating should be avoided, as it wastes water. If there is only dry food, it is better not to eat, as water is necessary for digestion. For severe cases of dehydration where fainting, unconsciousness, or other severely inhibiting symptom is present (the patient is incapable of standing or thinking clearly), emergency attention is required. Fluids containing a proper balance of replacement electrolytes are given orally or intravenously with continuing assessment of electrolyte status; complete resolution is the norm in all but the most extreme cases.
Avoiding dehydration
Dehydration is best avoided by drinking plenty of water. The greater the amount of water lost through perspiration, the more water must be consumed to replace it and avoid dehydration. Since the body cannot tolerate large deficits or excesses in total body water, consumption of water must be roughly concurrent with the loss (in other words, if one is perspiring, one should also be drinking water frequently). Drinking water beyond the needs of the body entails little risk, since the kidneys will efficiently remove any excess water through the urine with a large margin of safety.
A person's body, during an average day in a temperate climate such as the United Kingdom, loses approximately 2.5 litres of water. This can be through the lungs as water vapor, through the skin as sweat, or through the kidneys as urine. Some water (a less significant amount, in the absence of diarrhea) is also lost through the bowels. In warm or humid weather or during heavy exertion, however, the water loss can increase by an order of magnitude or more through perspiration; all of which must be promptly replaced. In extreme cases, the losses may be great enough to exceed the body's ability to absorb water from the gastrointestinal tract; in these cases, it is not possible to drink enough water to stay hydrated, and the only way to avoid dehydration is to reduce perspiration (through rest, a move to a cooler environment, etc.).
A useful rule of thumb for avoiding dehydration in hot or humid environments or during strenuous activity involves monitoring the frequency and character of urination. If one develops a full bladder at least every 3-5 hours and the urine is only lightly colored or colorless, chances are that dehydration is not occurring; if urine is deeply colored, or urination occurs only after many hours or not at all, water intake may not be adequate to maintain proper hydration.
When large amounts of water are being lost through perspiration and concurrently replaced by drinking, maintaining proper electrolyte balance becomes an issue. Drinking fluids that are hypertonic or hypotonic with respect to perspiration may have grave consequences (hyponatremia or hypernatremia, principally) as the total volume of water turnover increases.
If water is being lost through abnormal mechanisms such as vomiting or diarrhea, an imbalance can develop very quickly into a medical emergency. In fact, the main mechanisms through which diseases such as infantile diarrhea and cholera kill their victims are dehydration and loss of electrolytes.
During sports events, water stops and water breaks are provided to avoid dehydration of athletes.
See also
- Hypovolemia, a depletion of blood volume that can be caused by dehydration
- Safe water
- Water intoxication
- Water therapy
References
- Ira R. Byock, M.D., Patient Refusal of Nutrition and Hydration: Walking the Ever-Finer Line. American Journal Hospice & Palliative Care, pp. 8-13. (March/April 1995)
Notes
- ^ Dehydration Symptoms - Benefits of Drinking Water - Signs of Fluid Imbalance
- ^ Bean, Anita (2006). The Complete Guide to Sports Nutrition. A & C Black Publishers Ltd., pp. 81-83. ISBN 0713675586.
- ^ http://faculty.washington.edu/kepeter/118/notes/pdf-set5/118water-bal-06.htm
- ^ "Healthwise Handbook," Healthwise, Inc. 1999
External links
- Water requirements in adults
- Definition of dehydration by the U.S. National Institutes of Health's MedlinePlus medical encyclopedia
- Rehydration Project at rehydrate.org
| |||||||||||
Categories: Metabolic disorders | Electrolyte disturbances | Nutrition | Causes of death
.
.
.